
COVID support and return to work training
OVID is harshly impacting every aspect of our lives: mental health, relationships, physical wellness, and family. In collaboration with our partners Workright, We’ve put
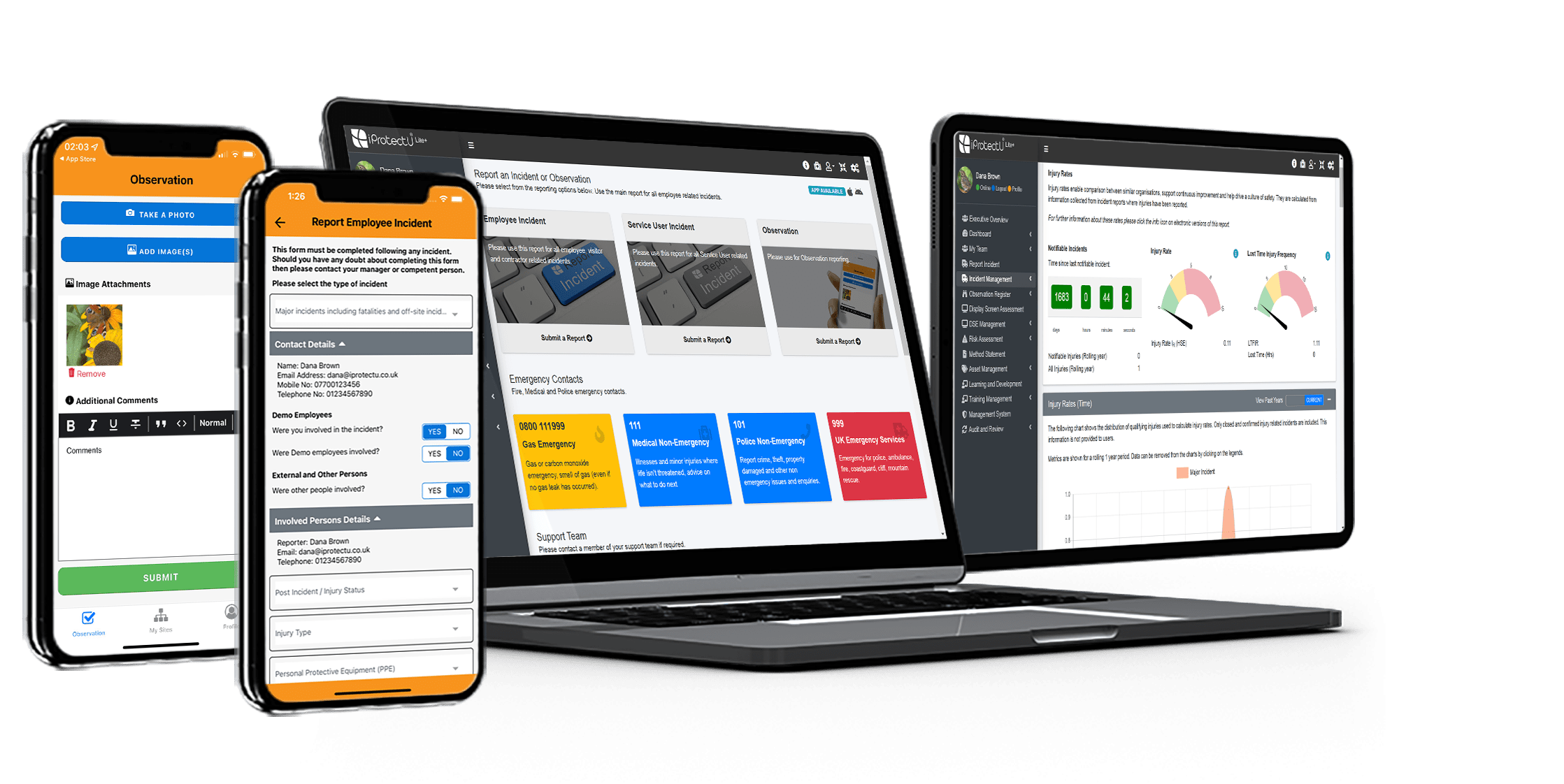
Lite with added extras
Includes ISO 9001 compliant document and asset management
Enterprise compliance
Everything you need in one fully integrated and configurable package
Our suite ISO Auditing modules and mobile apps, help businesses and organisations achieve compliance with ISO Standards.
Achieve ISO Certifications for your organisation, using our fully integrated ISO Auditing platform.
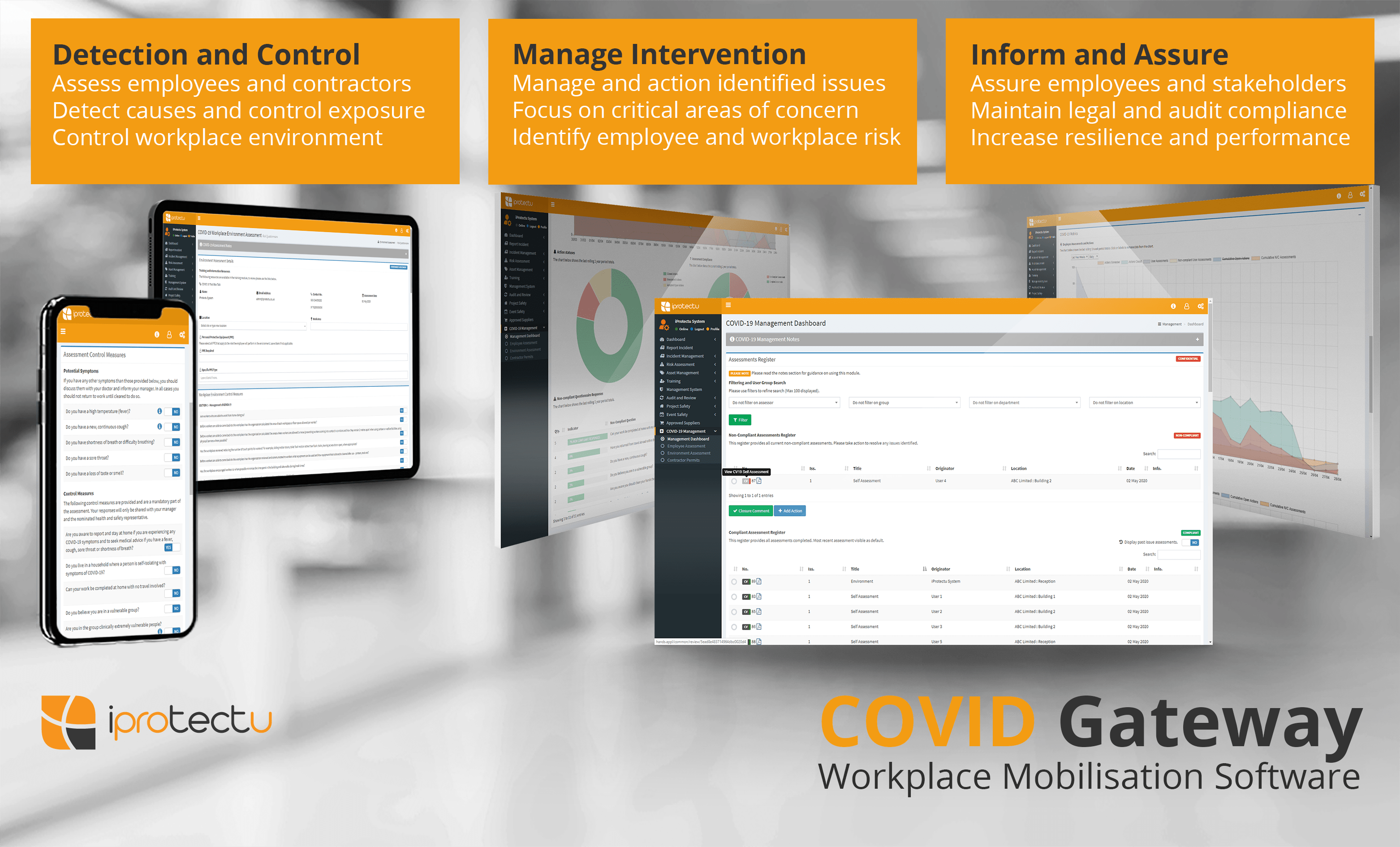
Health and Safety Software » COVID-19 Management » COVID Gateway and rapid antigen testing provide a holistic approach for employers

COVID Gateway Response is integrated into the already proven iProtectu health and safety management system. Complimented by management dashboards, coronavirus and hygiene video awareness training and risk assessment it is already enabling employers to bring their employees safely back into the workplace. With new technologies in rapid antigen testing this is further enhanced and enables a more holistic approach to COVID management for employers.
Antigen tests detect the presence of viral RNA, specific proteins on the surface of the virus, otherwise known as antigens. An RNA virus is a virus that has RNA (ribonucleic acid)1 as its genetic material. Detecting viral RNA usually requires taking a swab from the nose and throat and then analysing the specimen in the lab using the polymerase chain reaction (PCR) or by new technologies such as the Rapid COVID-19 Antigen Test Device.
Whilst there are significant differences in the two methods, the primary benefits of rapid testing methods are speed of distribution and price as they do not require complex and expensive laboratory equipment to perform the test.
Rapid testing is a useful measure in the fight against a virus and can help to identify people at the peak of an infection when virus levels in the body are at their highest. For a more detailed overview of what viral RNA load means, please view this Lancet journal publication2 by Gavin M Joynt and William KK Wu.
Rapid Antigen testing aims to see if the virus is detectable now. The test is taken to:
Whilst rapid antigen testing is not as sensitive as PCR methods which use laboratory testing, it is useful as part of a holistic approach to COVID management. Rapid antigen testing should be complimented by other strategies such as risk assessment, hygiene and awareness training, routine and regular hand washing, distancing, face coverings and employee monitoring.
Antigen tests are therefore a crucial part of mitigating transmission as we come out of lockdown. We need the ability to detect the carriage of covid-19 and respond to it rapidly. As people return to work and society tentatively re-opens, robust testing programmes as part of a return to work strategy will be key to reduce spread and improve confidence amongst employees and customers.
Test accuracy refers to two separate concepts: sensitivity and specificity.
Sensitivity concerns the false negative rate and is expressed as a percentage: out of 100 truly positive patients, how many are detected as positive by the test? The higher the sensitivity, the fewer the numbers of false negatives. In the USA, sensitivity is often called positive percent agreement (PPA).
Specificity concerns the false positive rate and is expressed as a percentage: out of 100 truly negative patients, how many are detected as negative by the test? The higher the specificity, the fewer the numbers of false positives. An example here would be if the test detects an antibody response to a different but related coronavirus. The individual would be informed that they have antibodies to covid-19 when in fact it would reflect infection with a different but similar coronavirus. In the USA, specificity is often called negative percent agreement (NPA).
Test results need to interpreted in context, the likelihood of a true positive or true negative will vary depending on the prevalence or how common the condition is within a population.
It is important to know when to take an antigen test, the highest, peak viral load is around the time of symptom onset. If using the test to diagnose, it is sensible to do an antigen test as soon as possible following symptom onset. Ideally the test should be performed within days 1-5 from onset of symptoms. Virus may be detected after this (and in some cases can be detected for a long time after) but the chances of detection decrease as the body clears the virus or it moves further down the respiratory tract (which requires a different sampling method).
What does a positive antigen test result mean?
A positive antigen test means that the covid-19 virus has been detected on the swab. These tests are highly specific, which means that the false positive rate is almost negligible. This means that the false positive rate is almost negligible. If the result is positive, it is highly likely to be true.
The test detects viral RNA and does not tell the difference between active viral infection and “dead” viral remnants. It therefore cannot distinguish between someone who is infectious (active virus) and someone who is not (dead virus shedding). To do this, you would need to extract the virus particles and try to infect cells to see if this is possible.
What does a negative antigen test result mean?
A negative result could mean one of several different things:
What does the future look like?
Point-of-care (POC) testing that can be self-administered and results available within 20 minutes, is already here and this is what is currently offered. Ideally, the test would be non-invasive and the results not too dependent on correct technique used.
Holistic approaches and workplace strategies that combine training, risk assessment and point of care antigen testing will reduce transmission, drive down the “R” (reproductive number) and improve safety in the workplace.
For employers trying to get employees back to work, reassuring them and their customers, these tests, software such as COVID Gateway and training will truly enable a safer return to work strategy.
References
https://en.wikipedia.org/wiki/RNA_virus
https://www.thelancet.com/journals/laninf/article/PIIS1473-3099(20)30237-1/fulltext

OVID is harshly impacting every aspect of our lives: mental health, relationships, physical wellness, and family. In collaboration with our partners Workright, We’ve put

In partnership with Private Harley Street Clinic (PHSC), iProtectu can provide COVID-19 Non Intrusive Saliva based Test Device. The test is provided by a world
This free resource is also available on our YouTube channel and can be used freely to raise awareness in the workplace.
Chemical safety management is a crucial investment in the health and wellbeing of your employees

iCertifyU provides FREE Administering Medication Awareness (in schools) training. Download the App from the App

In a world brimming with chemicals, from industrial solvents to cleaning products, understanding their potential
The EU AI Act will soon be formally adopted and is expected to come into

Leadership plays a crucial role in shaping an organisation’s OH&S culture and driving the successful
In today’s workplace, where operations are becoming increasingly complex and data-driven, technology plays a large
Arrange your demonstration
Let us show you how we can transform your compliance management
Choose a date and time for your demo (no obligation) and we will be in touch.